In early 2020, the COVID-19 pandemic just began to hit the United States. In anticipation of an emergency ventilator shortage, a group of engineers and scientists at MIT created a web page asking for help in designing and providing automated ventilators. There was predicted to be a 300,000-700,000-unit shortage of ventilators in just the United states alone. Coupled with the shortage would be rising costs for the few ventilators that would remain. There was even the concern if automated ventilators were even helpful to COVID-19 patients.
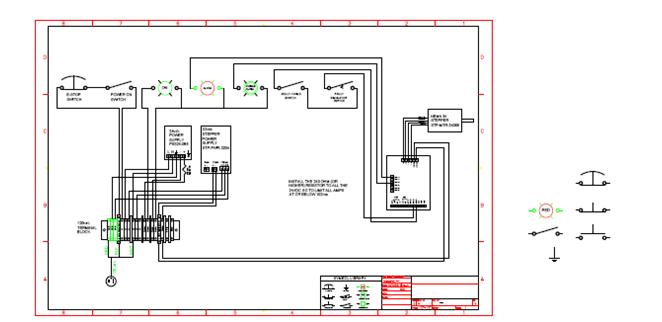
ANCORP decided that we should help. Our president, Daniel Vaudreuil, called a meeting of some of our engineers and asked them to construct a ventilator. Or, more specifically, a device that can automatically pump the ventilator to reduce both human interaction with a sick patient and to free up hospital staff. Glen Chaisson, along with the help of interns Sana Marrero and Drew Vaudreuil, created an improved ventilator.

MITs design had a ventilator that placed a device in the throat of the patient to measure their oxygen. This is a very risky method, so instead our team purchased an FDA ventilator that only pumps air into the mouth and designed a stepper motor that can be programed to pump air for various increments of time. The system was also designed with a failsafe that measured pressure inside the lungs and would stop automatically if there was too high pressure. It also was able to adjust pumping for people of various sizes.
Fortunately, the US was able to mass produce ventilators and did not see a mass overcrowding of hospitals. Even though our design was never used we are glad to know ANCORP will always be around to empower science and technology.
MIT Vent specifications:
- Respiratory Rate (RR) (breaths per minute): between 6 – 40. Note that the low RRs of 6 – 9 are only applicable to Assist Control.
- Tidal Volume(TV) (air volume pushed into lung): between 200 – 800 mL based on patient weight.
- I/E Ratio (inspiratory/expiration time ratio): recommended to start around 1:2; best if adjustable between range of 1:1 – 1:4*.
- Assist Control is based on a Trigger Sensitivity: When a patient tries to inspire, they can cause a dip on the order of 2 to 7 cm H2O, with respect to PEEP pressure (not necessarily equal to atmospheric pressure).
- Airway pressure must be monitored continually. Maximum pressure should be limited to 40 cm H2O at any time
- Plateau pressure should be limited to max 30 cm H2O.
- The use of a passive mechanical blow-off valve fixed at 40 cm H2O is strongly recommended. This is integrated into most manual resuscitators.
- Clinician require readings of plateau pressure and PEEP (refer to Clinical tab).
- PEEP of 5–15 cm H2O required; many patients need 10–15 cmH2O.
- Failure conditions must result in an alarm and permit conversion to manual clinician override, i.e. if automatic ventilation fails, the conversion to immediate ventilation must be immediate.